Validating Operational & Financial Assumptions Across the Lifecycle of Long-Term Capital Projects
With the construction of new hospitals and other major healthcare capital projects spanning five to 10 years from the initial plan through construction and occupancy, it’s important to prepare for the reality that circumstances will change over a long project lifecycle.
By Katherine Kay Brown, MSN, RN, and Terri Palazzo, MSN, RN, FACHE
With the construction of new hospitals and other major healthcare capital projects spanning five to 10 years from the initial plan through construction and occupancy, it’s important to prepare for the reality that circumstances will change over a long project lifecycle. Potential changes include shifts in community demographics and market dynamics, changes in payer reimbursement, rapid advances in technology, and changes in construction materials. Volume projections may also change significantly in that time, leading to different space requirements, shifting original budgeting and staffing assumptions as well.
Based on our deep experience, our Operational Readiness team understands how to make sense of all that is needed to operationalize a new facility to provide exceptional patient care from “Day One.” Operational readiness touches everything, including daily operations to staffing and supplies, quality care metrics, regulatory requirements, human resources forecasting and recruitment. We prepare organizations to be fully operational upon opening a new or renovated healthcare facility.
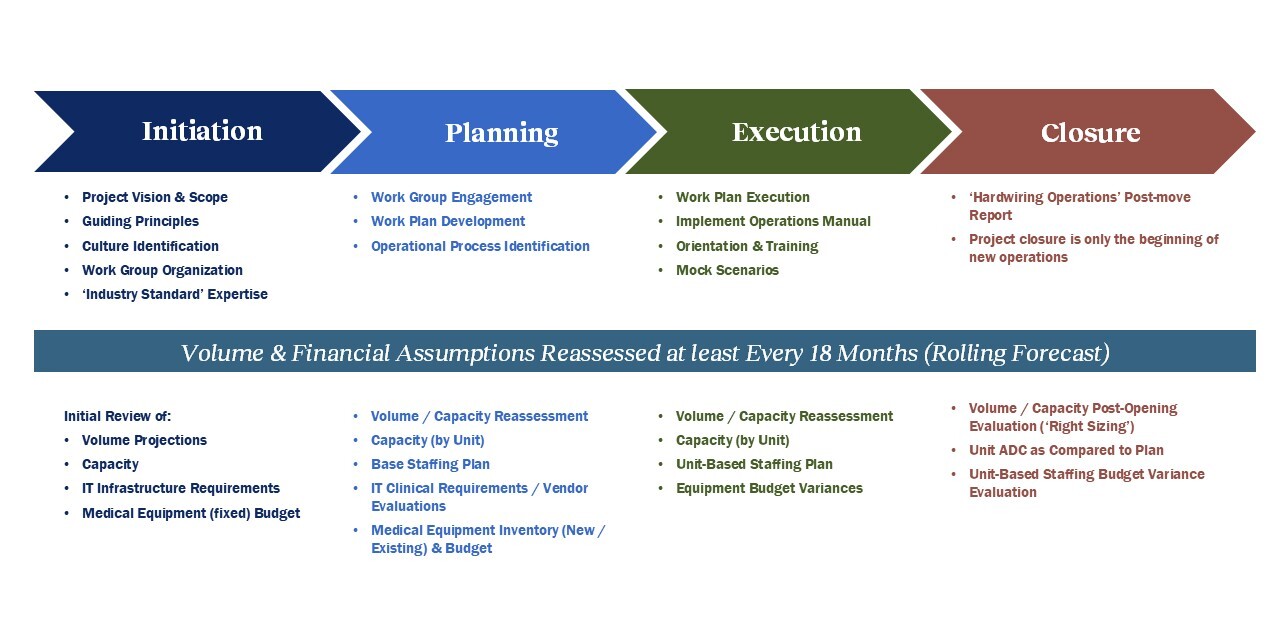
Here we offer an overview of our operational readiness approach, including six big questions that our team recommends revisiting throughout the project lifecycle. Revisiting initial assumptions helps ensure that when your facility opens, it fulfills your organization’s needs on “Day One” and well into the future.
Question #1: What Can Your Healthcare Market Support?
All major healthcare capital projects start with a market review that considers what a given market can support over the next decade and beyond. We recommend that healthcare organizations begin by consulting ten-year forecasts related to services including outpatient procedures and office visits, or acute and inpatient care.
Community demographics have the potential to change over the course of a project lifecycle, not to mention over the 50+ years that a hospital facility will serve the community. We recommend that healthcare organizations reassess volume and financial assumptions at regular intervals as the project progresses, no more than 18 months or with a rolling forecast. This allows you to ensure that the facility being built aligns with stakeholder goals and to catch important market changes so you can adjust if necessary.
Question #2: Who Are Your Competitors, and How Do They Influence Volume Assumptions?
Your competition is another variable that has the potential to change over the course of a long project lifecycle. For example, did a new player enter the market? You must know—and should reassess—the volumes that competing providers see in the service lines you hope to build or expand with the addition of your new facility. We have found that competition may come from sources outside traditional hospitals, such as urgent care facilities.
Consider this example of a hospital that has a major emergency department (ED) renovation and expansion project underway. Multiple urgent care facilities recently opened in the community, which reduced the hospital’s volume of low-acuity patients, or those with an emergency severity index (ESI) of 4 or 5. This hospital originally planned for a fast track or vertical care area with 24 bays designed to accelerate care and discharge of low-acuity patients. By monitoring patient acuity in the vertical care bays, the hospital determined that more than a third of patients in vertical care had an ESI of 3, suggesting that they had multiple comorbidities, such as diabetes or COPD. Even if the patients arrived at the ED with a minor problem, they were still likely to need a higher level of care. Based on this data, the hospital organization chose to increase the number of acute and critical care beds to accommodate these patients and reduce the fast-track bays by 30 percent.
Question #3: Do You Need to Adjust for Changes in Reimbursement or Regulatory Changes?
Successful capital projects not only re-evaluate initial volume assumptions to ensure that they still align with the strategic direction of the organization, but also the dynamic healthcare market.
Changes in reimbursement can alter financial forecasts. Consider the case of ophthalmology, which has shifted to a community-based ambulatory model and has therefore lowered reimbursements. In some facilities, it has become more difficult to recoup the cost of new instruments for cataract surgeries.
In contrast, changes in medical recommendations may increase volumes for other service lines, such as the 2021 decision by the U.S. Preventive Services Task Force to lower the age of first screening colonoscopy to age 45. Depending on your demographics, this increased screening can increase your gastrointestinal surgical volume, impacting demand on ORs.
Question #4: Do You Have Enough Physicians and Support Staff?
Staffing considerations are key to operational readiness and a project’s success. If you are considering the expansion of a service line but do not have enough physicians to perform the procedures, your capital project will not succeed. Here’s just one example: A hospital may wish to increase patient access to a particular surgery, but the ongoing shortage of anesthesiologists can limit its ability to offer those surgeries in your hospital.
We work with healthcare organizations to develop a provider network that is correctly sized to support expected market share. If you would like to grow a particular surgical offering or other specialty, hiring surgeons/specialists is an important step. But it is also necessary to consider the other staff members who provide a foundation to the surgeon’s work. The growth of that service line depends on hiring additional primary care physicians, who refer patients to see specialists, as well as adequate imaging staff, who offer an important step on the road to diagnosis and surgery.
We’ve seen some healthcare organizations make the mistake of thinking that because new space will not generate new patient volume in the first year or two after opening, no new staff is needed. But this is flawed logic; the reality is that more square footage means more support staff for facility cleaning and maintenance.
We also urge organizations to plan for hiring to take more time than expected. Healthcare has one of the longest time-to-fill rates of any industry, due in part to nurse and physician shortages and competition for candidates. The process can be further slowed if your human resources team does not yet have a reliable talent pipeline, which can take time to develop. Also, be prepared to provide training and orientation to a large influx of new staff will tax your human resources and education teams.
Question #5: Can You Accommodate Rapid Technological Change?
When planning a facility that will open to patients in five to 10 years, it is important to acknowledge the speed at which technologies evolve. We can expect AI and other disruptive technologies to play a growing role in healthcare settings. As a result, we advise keeping plans flexible and holding regular technology reviews to consider how tech will work with staff and patient workflows. This will help ensure that a long timeline does not result in a technologically outdated facility.
When designing new spaces, organizations must plan infrastructure that allows for expanding WiFi and power needs to enable inevitable advances in the future. You might also consider leasing equipment to avoid spending scarce capital dollars on hardware that may quickly grow obsolete.
Plan to test all new technologies before opening, preferably within your current environment. If a test run is not possible, or if you are designing for future technology that does not yet exist, build additional time into the project schedule to allow for testing and training. And rely on a Patient Advisory Committee to learn what experience patients want from hospital technologies, including the increasingly common “smart room” amenities. We find that too many decisions are made for hospital staff and not for the patient.
Question #6: Have You Prepared Your Team to Mobilize?
Not only does operational readiness require revisiting core budgeting and staffing assumptions, but it also involves activating people and processes specific to the new facility. By working closely with clinical and operational leaders, you can shape effective patient and staff workflows and support the department workflows needed for efficient, safe patient care in the new facility.
We regularly help organizations plan orientation and training curricula and stress the need to build in sufficient time for testing and training. This step ensures that staff have the required skills and competencies to deliver excellent care. We suggest using tools such as mock scenarios that focus on code blue, stroke alert, and mass transfusion drills, which help staff prepare for medical events that put patient lives at risk. We also recommend that teams run through routine patient and staff workflows. Such drills ensure that no matter how long a capital project has taken from start to finish, all staff are fully equipped for the first patients to arrive on Day One.
This article is based on a 2025 ACHE Congress on Healthcare Leadership presentation by Katherine Kay Brown, MSN, RN; Melody Dickerson, DNP, RN, FACHE, CENP, CPHQ, and Terri Palazzo, MSN, RN, FACHE. Katherine and Terri are Operational Readiness Executives with Hammes Healthcare who have collectively managed the transition to more than 40 new or renovated healthcare facilities over their careers.