Balancing Service Lines Across a Geography: A Strategic Imperative for Evolving Health Systems
Health system executives must confront a critical operational challenge: determining what services should be offered where—and why. The goal isn’t to reduce services indiscriminately, but rather to balance service line distribution across a market to increase access, improve quality, and lower cost.
By Michael Romano
Introduction: The Next Chapter in Health System Evolution
Over the past decade, the American healthcare landscape has been transformed by merger and acquisition (M&A) activity – two-thirds of all hospitals and 75% of all hospital beds in the U.S. are now system-affiliated. Once regionally focused, modestly sized hospital systems have rapidly grown into sprawling networks of facilities across expansive geographies.
Yet, despite the trend toward system aggregation, many systems are still operating in a decentralized, pre-integration mode, particularly when it comes to their service line strategies.
The Service Line Rationalization: Greater Access, Higher Quality, Lower Cost
Health system executives must now confront a critical operational challenge: determining what services should be offered where—and why. The goal isn’t to reduce services indiscriminately, but rather to balance service line distribution across a market to increase access, improve quality, and lower cost. Take, Labor and Delivery (L&D) as an example:
- Published studies suggest that “deliveries at high-volume obstetric hospitals are associated with improved infant and maternal outcomes.”
- Robust L&D programs include subspecialty support like maternal-fetal medicine and neonatology, Level III NICU services, and specialty-trained staff to support these programs.
- The fertility rate in the U.S. dropped to an all-time low in 2024.
- The physician subsidy for a 24/7 laborist and neonatologist coverage model at a typical community hospital could exceed $1.5-$2 million or more per year.
These facts taken together suggest that a community-based health system offering L&D in more than one location should consider consolidating services, but only if done thoughtfully and transparently.
Not a One-Size-Fits-All Strategy
A strategic misstep is assuming that every facility within a health system should offer the same suite of services. Instead, systems should embrace differentiation. One campus might become the orthopedic destination. Another might specialize in cardiovascular care. A third might serve as the central hub for complex maternity cases. Each location plays a role in the broader strategy, contributing to system strength through specialization—not replication.
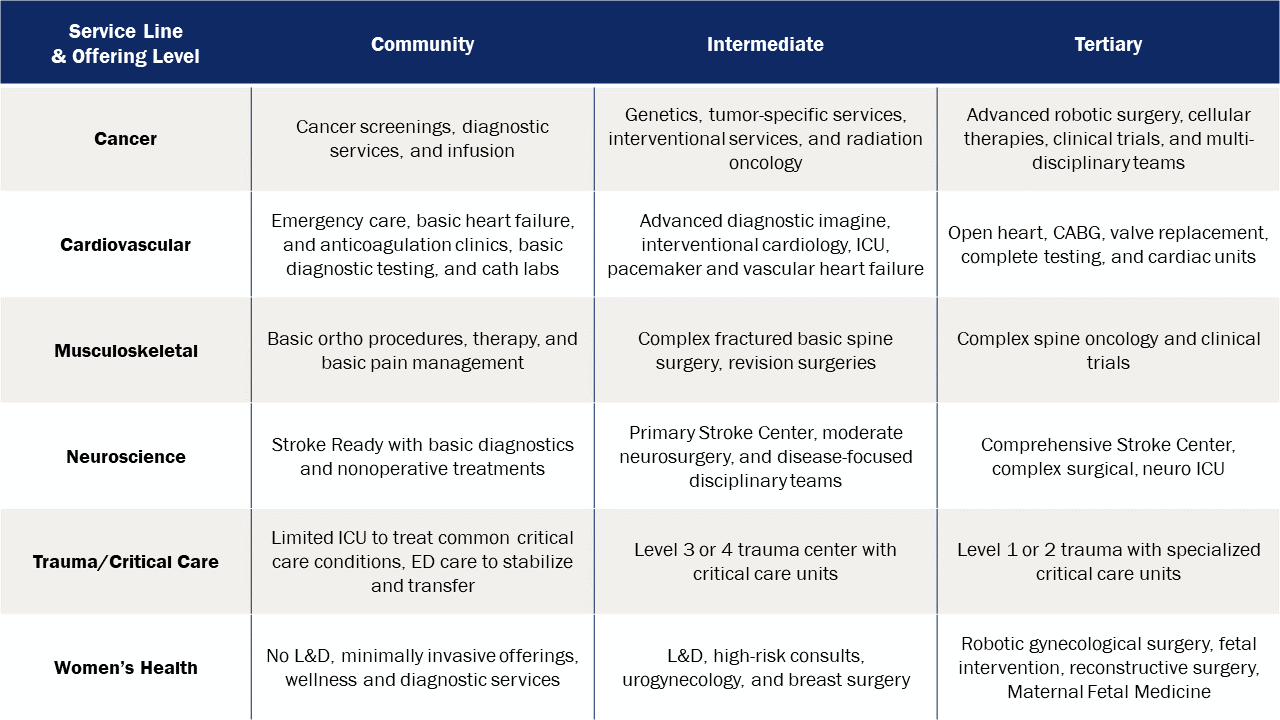
It's also important to understand that balancing service lines is not a “yes/no” question but, rather, should be viewed across a continuum for each location. In the table below, every acute care site in the same system may not need tertiary-level care for neuroscience or cardiovascular service lines.
There are several benefits to service line rationalization, for example, reduced congestion at larger system campuses and positioning systems to respond more nimbly to population growth in suburban corridors without overloading central facilities already at or near capacity. Campus specialization also enables provision of care closer to home, which demonstrates a commitment to community-based care and aligns with evolving patient expectations and payer models that prioritize value.
A Framework for Strategic Service Line Balancing or Rationalization
While there is no one-size-fits-all model, there are proven steps that can guide service line strategy:
- Conduct a geographic market analysis: Understand where your patients are, how they move through your system, and what the competitive landscape looks like.
- Embrace repatriation: Closer to home is better if the care is the same.
- Assess volume and quality metrics by service line: Determine which facilities are delivering high-quality care at scale and which are underperforming.
- Develop a service line matrix by campus: Define clear roles for each facility—anchor, specialty hub, community access point, etc.
- Align physician staffing with strategic goals: Build service lines around sustainable staffing models, not individual site preferences.
- Engage stakeholders with transparency: Communicate the rationale behind service shifts clearly to community leaders, staff, and patients.
- Develop critical thresholds: Define clear expectations and measures that create future pathways for increasing service line levels at care sites.
Conclusion: From Aggregation to Optimization
The era of rapid M&A has given way to a new phase in healthcare system strategy and evolution: one where success will be defined not by size alone, but by how systems strategically deploy their resources to improve access while delivering higher quality care at a lower cost. Balancing service lines across a geography is not only a logistical necessity but a strategic imperative.
By making data-informed, patient-centered decisions about where to invest, expand, or consolidate, health system executives can chart a course toward long-term sustainability, clinical excellence, and community trust.
References:
JAMA Netw Open. 2021 Oct 8;4(10):e2125373. doi: 10.1001/jamanetworkopen.2021.25373
AMGA, “New survey finds medical group operating costs continue to outpace revenue,” press release, Dec. 18, 2023.
AHA, https://www.aha.org/system/fil...